Exercise Associated Muscle Cramps (EAMC)
- by Joanna Blair
- •
- 28 May, 2018
- •

Unsurprisingly, after runners had been out in the unforgiving heat (23.2 degrees) for more than 3-6+ hours, various suffered fromthe condition afterwards and has been this month's main topic of study.
Congratulations must be given to every runner who participated and completed the race that day. Even for the experienced runners, the unexpected heat put them through their paces. It was inspirational to meet runners from up and down the country of all abilities running for a great cause, and to soldier on to the finish line despite the baking conditions and gasping for fluids with drinks stations running out of water between miles 15 to 19! Utmost respect, and the man of the match for me was the superb (but barking) runner who completed the course whilst dressed in a fluffy dinosaur costume for the charity.
Exercise Associated Muscle Cramps (EAMC), What Is It, Who is Prone to Experiencing Them and Why Do They Occur?
The incidence of EAMC can occur suddenly with no warning and last for several days, most last for 1-3 minutes but some athletes can complain of symptoms for lasting up to 8 hours post exercise, a period otherwise known as the 'cramp prone state' (9, 7).
Risk Factors
- The elderly.
- Long history of running.
- High Body Mass Index.
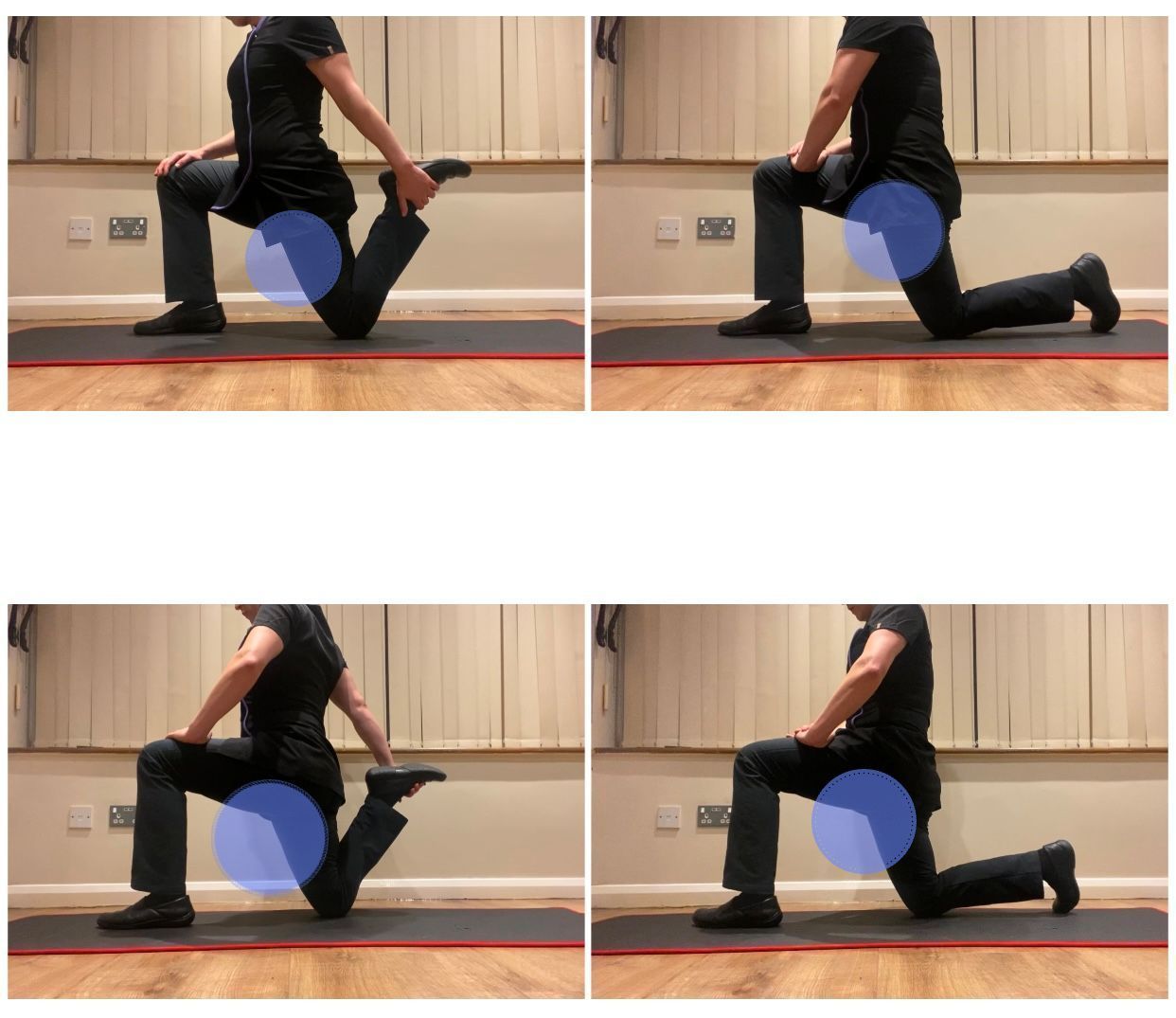
- Shorter daily stretching time.
- Irregular stretching habits.
- Family history of cramping (genetic predisposition).
- Competing at a higher exercise intensity.
- Running conditions; high intensity, long durations of running, hills or inclines.
- Carbohydrate, glycogen depletion.
- Poor biomechanics or running gait.
- Hilly terrain.
- Lack of
adequate massage before and during a gam/ exercise.
The Electrolyte-Balance-and-Dehydration Theory
The electrolyte imbalance theory explains how excessive sweating leads to reduced concentrations of serum electrolytes, in particular sodium (Na+) and chloride (Cl-), but also calcium (Ca2+), magnesium (Mg) and potassium (K+) (8). A whole body sodium deficit develops after a long bout of vigorous exercise and when a loss of electrolytes significantly exceeds salt intake(8). Interestingly, it is estimated that a 20-30% loss of sodium has been linked to severe muscle cramping (8).
The dehydration theory suggests that excessive sweating reduces plasma volume in the blood which causes water from the interstitial fluid compartment to shift to the intravascular space by osmosis (9). As sweating continues, the interstitial fluid compartment contracts which causes neuromuscular junctions (in muscles heavily used) to become hyperexcitable and spontaneous discharges of motor neurons cause muscle cramping (9).
A useful video to show the difference between hypo, iso and hypertonic environment states in cells:
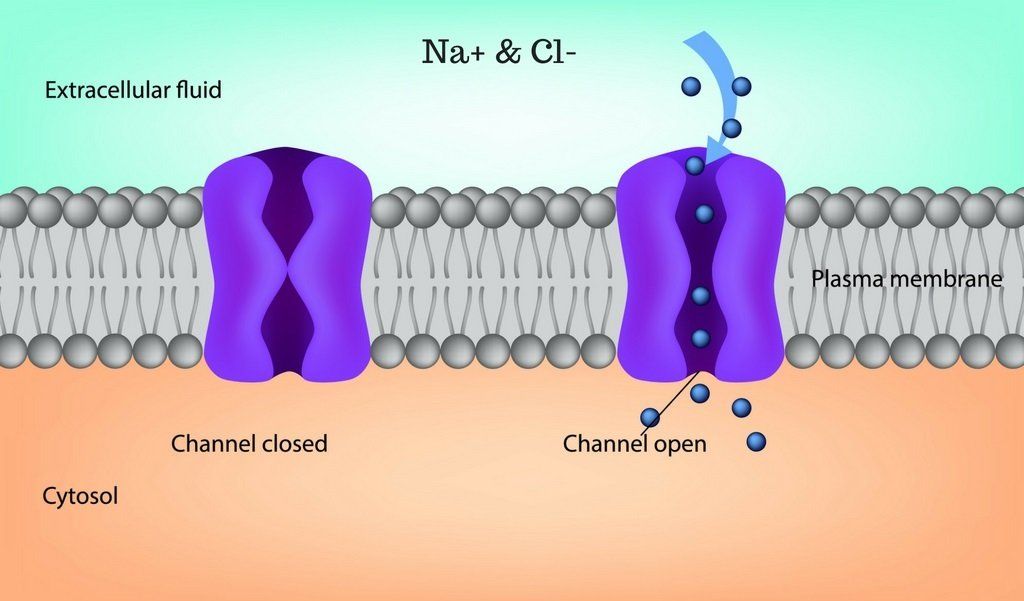
Critique To the Dehydration Theory
The electrolyte imbalance theory suggests that a lack of sodium, potassium and magnesium from sweating causes electrophysiological changes at the muscle which leads to cramping (6, 8). As discussed above, the problem with this theory is that dehydration leads to elevated serum electrolyte levels and drinking excessive amounts of water will lower serum electrolytes, but neither scenario had an increased incidence of EAMC (4, 8). Schewellnus (2009) highlight that eating bananas or ingesting salt pills will not prevent muscle cramps either.
Altered Neuromuscular Control Theory
The altered neuromuscular control theory explains how muscle fatigue disrupts the normal functioning of two important muscle proprioceptors that help regulate muscle length and tone. Golgi Tendon Organs (GTOs) are receptors located in muscle tendons close to the muscle attachments which are activated by muscle stretch or contraction and transmit information about muscle tension (7).
The receptors can be stimulated either by contraction or stretch, however, muscle contraction is more effective in initiating active potentials (APs) in GTOs (7). Stimulation of the GTO causes afferent neurons to transmit signals to the spinal cord and cause contracted muscles to relax which is opposite to muscle spindle receptors, causing muscles to contract (9).
Muscle fatigue develops when there is an increased firing rate or activity of muscle spindles and reduced activity of GTOs. The central nervous system (CNS) regulates the loading of muscle (stretch) via alpha motor neurons which modulate spindle activity and make the transition from stretch of muscle to contraction smoother (2). Muscle cramps can be viewed as a consequence of a sustained alpha motor neuron dischargewhich occurs when the enhanced excitatory activity of the muscle spindle that triggers an involuntary muscle contraction is unopposed by Golgi tendon organs which are designed to inhibit this muscular response (9). As a result, excitatory activity from the muscle spindles triggers an intense and sustained involuntary muscle contraction (1).
Differential Diagnosis
- Sudden in onset from exertion-related activity
- Localised
- Asymmetric
- Responds well to passive stretching and massage
Muscle cramps that happen as a result of exertional heat usually:
- Progressively develop over time
- Cramping can become more severe and widespread (often bilaterally)
- Muscle spasms are intermittent.
Recovering and Preventing Muscle Cramps
For muscle cramp cases that might be related to an electrolyte deficit, ingestion of a high-salt solution has been proven effective to prevent muscle fasciculations and beneficent effects can be seen in just a few minutes as the beverage is rapidly absorbed (1.). Overall, maintaining hydration and sodium balance is the proven effective prevention strategy for exertional heat cramps in workers and athletes during their physical activities.
References:
(4.) Jung, A. P., Bishop, P. A., Al-Nawwas, A. and Dale, B. R. (2005) Influence of Hydration and Electrolyte Supplementation on Incidence and Time to Onset of Exercise-Associated Muscle Cramps, J Athl Train. 40(2): 71–75.